
Illinois Treatment Center

MDMA and Molly are illicit lab-made drugs that have stimulant and hallucinogenic effects. Some researchers classify these drugs as psychedelics...

Is Ketamine a Horse Tranquilizer?
The question “Is ketamine a horse tranquilizer?” is a common one, and it’s easy to see why: ketamine has a...

Why Take Low-Dose Naltrexone at Night?
If you are trying to become sober, medication-assisted treatment (MAT) may be able to help. Naltrexone, an opioid antagonist, can...

Ecstasy vs MDMA
Many intertwine the terms Methylenedioxymethamphetamine (MDMA) and ecstasy, but they’re different in their own right. However, one thing both of...

How Much Is Ketamine Therapy?
Despite being relatively new, ketamine therapy for treatment-resistant depression is already gaining massive popularity. Back in 2015, there were around...
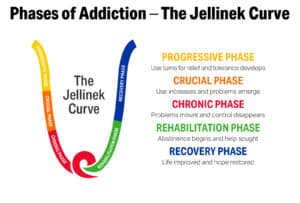
What Is the Jellinek Curve?
Alcoholism is a serious medical condition and is one of the most common addictions worldwide. While each person experiences it...

Is NyQuil Addicting?
NyQuil is one of the most popular medications in the United States, and it is used to relieve common cold...

Is Prozac Addictive?
In modern times, Prozac is one of the most frequently prescribed medications for mental health. Also known by its generic...

Understanding Pink Perc 10 (K 56 Pill)
“Pink Perc 10” is the short name for Percocet 10 mg tablets. Percocet is a brand-name prescription opioid that is...

Can I Get Addicted to Phentermine?
Phentermine is a generic pharmaceutical medication. Physicians prescribe phentermine to help overweight and obese patients lose weight. The drug is...
Real Reviews from Real Clients
At Illinois Recovery Center, prioritizing client care is our utmost concern. As you enter our facility, expect a heartfelt greeting from each member of our staff! We are committed to providing outstanding addiction treatment services and cultivating a supportive atmosphere conducive to sustained recovery. But don't just take our word for it... read what our clients have to say!



